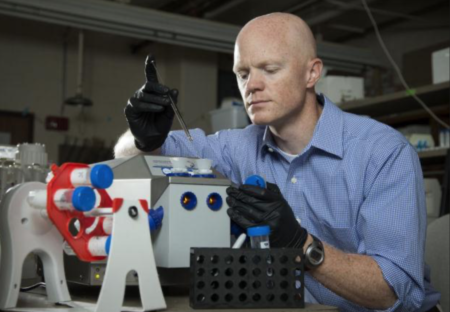
A few days ago, I reviewed Dr. Benjamin Bikman’s first book, Why We Get Sick. This book offers useful information for people who are striving to remain healthy. Since it has been widely reported that people with chronic diseases tend to struggle more with the COVID-19 virus, it is helpful to know how to avoid some of these conditions. To learn more about Dr. Bikman’s background and research, continue reading.
You studied exercise science as an undergraduate and exercise physiology at the graduate level. How does this background knowledge add to your understanding of how activity levels affect insulin resistance?
I’m profoundly grateful for my background. By starting with exercise physiology, I was able to build my deeper knowledge of human metabolism on a firm foundation of applied science. Essentially, this enabled me to keep in mind that all the complexity of human metabolism needs to be kept in the context of the entire human body, not just a reaction in a cell.
Most people are unfamiliar with what a PhD candidate studies for a bioenergetics graduate degree. Can you briefly describe the parameters of this discipline and how this field of study helped you reach the conclusions that you shared in Why We Get Sick?
Bioenergetics was a very valuable degree for me to better understand nutrient biochemistry and the process whereby a cell, and the body by extension, converts energy in consumed nutrients to energy in a cell. So many biochemical reactions, and virtually all that are related to nutrients and food, are regulated by insulin. In other words, for human metabolism to function properly, the hormone insulin must itself work properly. Unfortunately, our modern lifestyle creates a perfect metabolic storm that both drives insulin up constantly, as well as disrupts its ability to regulate metabolic functions in cells.
What inspired your interest in cardiovascular and metabolic disease?
My initial interest in science was to better understand how the body responds and adapts to exercise. However, during the course of my master’s degree, my interests began to shift more towards obesity and related metabolic disorders. I believe I can track this to one moment.
Around 2004, I stumbled across a study published a few years prior that detailed the ability of fat cells to release hormones that promote inflammation. At that time, and to this day, people were studying how the role of inflammation is causing numerous problems, such as heart disease and diabetes. Realizing that fat cells directly contribute to this planted a seed of curiosity that I’ve been nurturing ever since.
What contributions do you hope to make to this field of study?
At the end of my career, I’d like to look back knowing that I contributed to people becoming increasingly aware of the pathogenic side of insulin. Too few people, including health practitioners, appreciate that insulin has a dark side. We all know that too little insulin causes problems (e.g., type 1 diabetes), but nobody talks about the dangers of too much insulin (e.g., type 2 diabetes, dementia, infertility, etc.).
Since your 2011 completion of a postdoctoral fellowship at Duke NUS Graduate Medical School, Singapore, can you identify any changes in your perspective on how to avoid insulin resistance? In other words, had your thinking changed much in the last decade?
The most pivotal shift in my thinking has occurred with regards to the role of diet in driving metabolic disorders, such as obesity and insulin resistance. Like so many others, I viewed these as purely problems of “energy balance”—that it was a simple matter of caloric mathematics. While I still believe calories are relevant, I very much believe that hormones, especially insulin, must be considered in the equation. Insulin tells the body what to do with the energy that it eats: whether to stores or use.
Your Bingham Young University biography states that you are currently exploring the contrasting roles of insulin and ketones as key drivers of metabolic function. Can you share anything about this research and what you hope to learn?
Insulin has a direct effect on how every cells uses energy. Essentially, insulin promotes energy storage. One way it does this is to slow the metabolic rate of cells, a phenomenon that is even detectable in the whole body; increasing insulin slows metabolic rate by up 20%. We recently published that insulin slows the metabolic rate in fat cells, which may contribute to the overall reduced metabolic rate. In contrast, ketones, which are by-products of fat burning, stimulates these same fat cells to have a higher metabolic rate. Indeed, when exposed to ketones, metabolic rate in human fat cells increases by 200%.
Medical doctors have told their patients for years to keep their cholesterol levels down in order to avoid heart disease. Can you explain why you feel that insulin resistance is a greater concern? (On page 23, you stated, “there is no single variable more relevant to heart disease than insulin resistance?”)
I realize this is a bold statement, but I believe it’s supported in the evidence. So much focus is spent on LDL cholesterol. However, if a person is insulin sensitive, having a high LDL level is meaningless with regards to the risk of having a heart attack. In contrast, even a low LDL won’t protect a person from a heart attack if they’re insulin resistant.
On page 20, you briefly mention your concerns about the use of statins. If a person stops taking statins, do the negative side effects remain or do they diminish after the drug is no longer taken?
The risk-benefit equation with statins involves several variables, including age, sex, and confirmation of atherosclerotic plaques in the heart vessels. If a person has little or no plaque, statins have very little benefit. Of the side effects related to statins, including increased diabetes risk, muscle pain, and more, I speculate that these are temporary.
Some doctors, like Dr. Dean Ornish and Dr. Joel Fuhrman, advocate a vegetarian diet. Can you elaborate further as to why you feel that high fat dairy products, meat, fish, and eggs should be part of a healthy diet?
I am an advocate of ancestral fats—the fats that our species has been eating since the beginning of time. At its simplest, we could define these as animal and fruit fats. The evidence supporting our consumption of animal fats is inarguable and, frankly, any attempt to claim otherwise is ridiculous.
With fruit fats, our ancestors would have simply needed to press the flesh of the fatty fruits (especially olives and coconuts) to obtain the oil. My defense of animal fats comes from the dozens of published clinical studies that compare low-fat diets to low-carbohydrate diets.
Importantly, the low-carbohydrate diets generally always skew towards more animal-sourced foods, including meat and eggs. Despite eating several times more saturated fat from animal products, the subjects adhering to a low-carbohydrate diet have the greatest drop in insulin levels, including favorable changes in glucose and blood lipids.
In Appendix A it states that seven fats and oils can be eaten until satiated. Is there a maximum amount that should be consumed per day?
No, I’m unaware of an upper limit with daily fat consumption. I would state, however, that there is also no need to aim for a daily target. Essentially, a person should eat fat with protein, with some additions in the form of butter or oils. This is an important point though—the best sources of protein for humans are eggs, dairy, and beef.
This is an inconvenient fact for some, but it’s reality. Importantly, these proteins sources come with fat. And science supports this duo—adding fat to protein actually helps the protein work better, at least with regards to muscle growth and health.
Plant proteins, in contrast, are inferior in every way. Despite the cultural trend and even obsession with soy and pea proteins, these are inferior sources of amino acids, and they come with serious considerations. Not only do these proteins carry anti-nutrients that actually partially block the body’s ability to digest and use the protein, but they also come with heavy metals, such as lead and arsenic.
Are you singling out the 16 fruits, listed in Appendix A, due to their high carbohydrate content? Does the carbohydrate content outweigh the nutritional value?
It’s a delicate issue to discuss the nutritional value of fruits, but the reality is that humans have no need of fruits whatsoever—they provide nothing essential. However! I’m not advocating people don’t eat them at all, but rather that they appreciate that the modern fruits are “sugar bombs”. Depending on the underlying insulin sensitivity of a person, fruits are something that can be enjoyed frequently or, in the case of someone with insulin resistance, rather infrequently.

Are your recommendations for people who are more likely to become insulin resistant due to age, ethnicity, genetics the same as for those who do not have an underlying predisposition?
Absolutely not. In fact, I outlined a study in my book that explored the efficacy of both low-fat and low-carb diets in people that were split into two groups based on insulin sensitivity. The insulin sensitive people benefitted equally from either diet. However, the insulin-resistant group experienced only a benefit from the low-carb diet.
Are the four pillars to your plan for keeping insulin low—control carbohydrates, prioritize protein, fill with fat, and watch the clock—on equal footing? In other words, should all four be adhered to equally?
What a great question…I’m not sure how to answer this. I think that fasting can make up for some diet errors. However, I’ve also seen fasting be abused as a sort of daily “binge and purge”. I believe #1 is the best to focus on—if a person is controlling the consumption of carbohydrates, the other three will tend to fall in place.
Does any of your research point to the possibility that there are individual differences in the way people react to carbohydrates? (For example, Eran Segal’s research suggests that a person’s genetics determines their response to foods.)
Yes—different people tolerate carbohydrates differently. Most often, these differences derive from inherent differences in insulin sensitivity. And inherent insulin sensitivity is a function of both genetics and environment. However, it’s really not possible to identify a specific genetic code or pattern that reveals one’s underlying susceptibility. Frankly, that was the purpose of the short quiz at the beginning of the book.
Here is a link to my review of Why We Get Sick.
DISCLOSURE
I received a complimentary copy of Why We Get Sick.
RELATED POSTS
Why We Get Sick: Showcases Linkage Between Insulin Resistance and Chronic Illness
Eat to Beat Disease and Glioblastoma
Should Glioblastoma Patients Investigate Radical Remission?
Can Your Diet Influence COVID-19 Immunity?
5 Ways to Improve Exercise Motivation
Perseverance Leads to Successful Recovery
How Do I Become Motivated to Live a Healthy Life
BIO
Sandra Bornstein is the author of May This Be the Best Year of Your Life. Sandra’s memoir highlights her living and teaching adventure in Bangalore, India. She was a licensed Colorado teacher who taught K-12 students in the United States and abroad. Sandra also taught college-level courses at Front Range Community College and the University of Colorado-Boulder.
In addition to reviewing books and interviewing authors, Sandra is an award-winning author and lifestyle and travel journalist. Many of Sandra’s travel stories appear on the For Readers Page. To follow Sandra’s travel adventures, visit TheTravelingBornsteins website.
Connect with Sandra